ROOPAK GOSWAMI
Shillong, Jan 13: In Meghalaya, where communities live in close-knit villages, an intriguing story of health and human connection is unfolding. Scientists are uncovering how social networks, rather than individual efforts or traditional health campaigns alone, are playing a pivotal role in combating malaria—a disease that has long plagued this region.

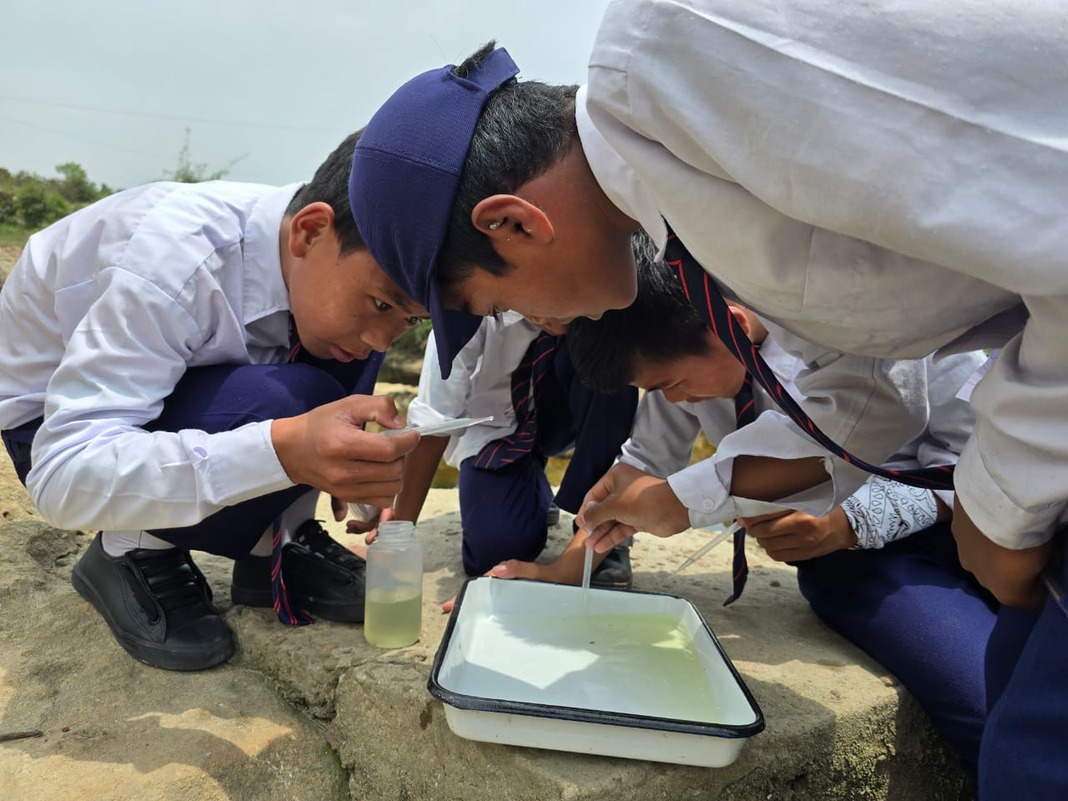
A study conducted across 10 rural villages in Meghalaya offers new insights into the power of social influence in driving public health outcomes. Researchers collected data from over 1,500 residents between 2020 and 2022, focusing on the adoption of eight malaria prevention techniques—ranging from the use of insecticide-treated bed nets to repellents and traditional methods like burning materials to ward off mosquitoes. The findings reveal that who you talk to about health in your village matters as much as if not more than, what you know.

The study was conducted by an interdisciplinary team of researchers, including Dr András Vörös from the University of Birmingham, Dr Elisa Bellotti from the University of Manchester, and contributors from institutions in India, such as the Indian Institute of Public Health Shillong and Martin Luther Christian University. Other collaborators included experts from New York University and Johns Hopkins Bloomberg School of Public Health. It was published in Scientific Reports, a peer-reviewed journal.
Social networks are increasingly recognized as important in explaining the adoption of single disease prevention behaviours The size (number of contacts) and composition of one’s network have been shown to matter for prevention behaviours related to HIV and the avoidance of alcohol and smoking. Social influence, adopting behaviour due to exposure to it in one’s network, also plays a role in the uptake of vaccination (e.g., HPV, influenza), HIV testing, and health-risk behaviours such as smoking, alcohol consumption, and substance use.

“Statistical network modelling reveals exposure to similar behaviours in one’s social network as the most important factor explaining prevention behaviours. Further, we find that households indirectly shape behaviours as key contexts for social ties. Together, these two factors are crucial for explaining the observed patterns of behaviour and social networks in the data, outweighing individual characteristics, opinion leaders, and social network size. The results highlight that social network processes may facilitate or hamper disease prevention efforts that rely on a combination of behaviours” the study says.
The study’s key revelation?
Villagers are more likely to adopt malaria prevention behaviours if others in their social network—friends, family, and neighbours—also practice these habits. This phenomenon, termed “social network exposure,” emerged as the single most significant factor influencing behaviour adoption. For each additional social connection adopting a prevention behaviour, the odds of someone else doing the same doubled.

The Household Factor
Households, the study found, are not just physical shelters but hubs of behavioural reinforcement. While shared living arrangements facilitate health discussions, the adoption of malaria prevention behaviour within households did not show a direct influence. This paradox highlights that while conversations start at home, the broader social web determines their impact.
Opinion Leaders and Missed Opportunities
Interestingly, health experts like government-appointed Accredited Social Health Activists (ASHAs) and tribal Traditional Healers, often seen as the cornerstone of health advocacy, had a surprisingly limited influence. The researchers suggest that while these figures provide valuable information, their effect pales in comparison to behavioural reinforcement from peers.

The Bigger Picture
For the first time since the start of malaria elimination efforts in India, local elimination may be within reach. “However, current control efforts rely solely on mass-administered interventions and include large-scale distribution of long-lasting insecticidal nets for beds, which was interrupted in India during the COVID-19 pandemic, and indoor residual spraying, which is met with high levels of refusal across the state,” the study says.
Our study suggests that these interventions could be complemented with targeted efforts that rely on social influence in interpersonal relations to increase the uptake of alternative prevention techniques. “Such efforts could support downstream elimination goals, including influencing the acceptance of a malaria vaccine. Future studies based on our approach could help to develop network-based strategies to promote multiple prevention behaviours for various infectious and non-communicable diseases. Looking beyond the scope of a single disease, examining a wider set of behaviours and beliefs could help to understand and exploit links between people’s long-term healthy lifestyles and short-term, targeted prevention behaviour” the study suggests.